Scarring alopecia, also known as cicatricial alopecia, is a distressing condition characterized by hair loss caused by inflammation, which leads to the destruction of hair follicles and their replacement with scar tissue. This disruptive process affects the normal hair growth cycle, resulting in permanent hair loss in the affected areas. Understanding the underlying mechanisms of scarring alopecia is essential for effectively addressing its impact on individuals’ lives.
Hair loss, especially when permanent, can have profound psychological effects, leading to feelings of self-consciousness, social withdrawal, and decreased self-confidence. The emotional burden associated with scarring alopecia can be overwhelming for those affected, affecting their relationships, professional opportunities, and overall well-being.
Early intervention plays a paramount role in managing scarring alopecia. By recognizing the signs and symptoms of this condition, individuals can promptly seek appropriate medical attention. Timely diagnosis and treatment can help prevent further hair loss and potentially reverse the progression of the disease. Moreover, early intervention significantly improves the chances of successfully managing scarring alopecia and minimizing its impact on one’s life.
Causes of Scarring Alopecia
Autoimmune Disorders
Autoimmune disorders play a significant role in triggering an immune response that attacks hair follicles, leading to scarring alopecia. In these conditions, the body’s immune system mistakenly identifies hair follicles as foreign and launches an immune attack against them.
Specific autoimmune conditions associated with scarring alopecia include discoid lupus erythematosus (DLE) and lichen planopilaris (LPP). In DLE, the immune response primarily affects the skin, resulting in round or disc-shaped patches of hair loss. LPP, on the other hand, causes inflammation and scarring of the hair follicles, leading to permanent hair loss.
Inflammatory Conditions
Chronic inflammation can also contribute to the development of scarring alopecia. Inflammatory conditions like folliculitis decalvans and central centrifugal cicatricial alopecia (CCCA) are closely linked to this type of hair loss.
Folliculitis decalvans is characterized by pustules and scarring, which can lead to permanent hair loss. It is believed to be caused by bacterial infections of the hair follicles. CCCA primarily affects the central scalp and is associated with prolonged inflammation and subsequent scarring of the hair follicles.
Genetic Factors
Genetic predisposition plays a crucial role in the development of cicatricial alopecia. Certain individuals may inherit genes that make them more susceptible to this condition. However, the specific genes and inheritance patterns associated with scarring alopecia are still being studied and understood.
Trauma or Injury to the Scalp
Physical trauma or injury to the scalp can also contribute to scarring alopecia. Any damage to the hair follicles can lead to inflammation and subsequent scarring, resulting in permanent hair loss. It is essential to protect the scalp from injuries, such as burns, scars, or surgical procedures, to minimize the risk of scarring alopecia.
Types of Scarring Alopecia
Understanding the distinct subtypes of cicatricial alopecia is critical for accurate diagnosis and appropriate treatment, emphasizing the significance of timely medical intervention and ongoing research to manage this complex condition effectively.
Discoid Lupus Erythematosus (DLE)
DLE is characterized by the presence of round or disc-shaped patches of hair loss. In addition to hair loss, individuals with DLE may experience redness, scaling, and scarring of the affected areas. If left untreated, DLE-related scarring alopecia can lead to permanent hair loss. Treatment options for DLE include topical corticosteroids, immunomodulatory medications, and sun protection.
Central Centrifugal Cicatricial Alopecia (CCCA)
CCCA primarily affects the central scalp, leading to progressive hair loss and scarring. It predominantly affects women of African descent, and the exact cause is still unclear. Diagnosing CCCA can be challenging, as it mimics other types of hair loss. Treatment options include anti-inflammatory medications, topical minoxidil, and hair transplantation.
Folliculitis Decalvans
Folliculitis decalvans is characterized by pustules, inflammation, and scarring of the hair follicles. This condition can result in permanent hair loss if not properly managed. Treatment options for folliculitis decalvans include antibiotics, topical corticosteroids, and oral immunosuppressive medications.
Lichen Planopilaris (LPP)
LPP is an autoimmune condition that affects the hair follicles, leading to red, itchy, and scaly patches on the scalp. Over time, LPP can cause scarring and permanent hair loss. Treatment options for LPP-related scarring alopecia include topical corticosteroids, oral immunosuppressive medications, and phototherapy.
Frontal Fibrosing Alopecia (FFA)
FFA primarily affects the frontal hairline, causing it to recede and leading to cicatricial alopecia. The exact cause of FFA is still unknown, but hormonal and genetic factors may play a role. Treatment approaches for FFA-related scarring alopecia include topical corticosteroids, oral medications, and hair transplantation.
Other Less Common Types of scarring alopecia
Less common types of scarring alopecia include dissecting cellulitis and pseudopelade of Brocq. Dissecting cellulitis is characterized by painful nodules, abscesses, and scarring, while pseudopelade of Brocq leads to patchy hair loss and scarring. These conditions require specialized management and treatment approaches.
Prevalence and Demographics
The prevalence of scarring alopecia varies worldwide, with estimates suggesting that it affects a small percentage of the population. However, accurate data on global incidence rates are limited due to underdiagnosis and misclassification of cases. Further research is needed to determine the true prevalence of scarring alopecia.
Scarring alopecia can affect individuals of all ages, including children and adults. While it can occur at any age, certain types of cicatricial alopecia may have a predilection for specific age groups. For example, DLE-related scarring alopecia is more commonly seen in adults, while CCCA is more prevalent in middle-aged women. The impact of cicatricial alopecia on quality of life can be significant, regardless of age.
Gender disparities in the prevalence of scarring alopecia exist, with certain types being more common in either males or females. For instance, CCCA predominantly affects women, while folliculitis decalvans is more frequently seen in men. Understanding these gender differences is crucial for accurate diagnosis and appropriate management.
Scarring alopecia may exhibit ethnic or racial differences in its occurrence. For example, CCCA is more prevalent in individuals of African descent, while DLE is more commonly seen in individuals of African, Asian, and Hispanic descent.
Common Symptoms of Scarring Alopecia
Understanding the symptoms and diagnostic procedures of scarring alopecia is crucial for accurate identification and management of the condition. By recognizing the various patterns of hair loss, scalp inflammation, changes in hair texture, and utilizing diagnostic tools such as scalp biopsy, blood tests, and dermoscopy, healthcare providers can provide comprehensive care to individuals affected by scarring alopecia.
Hair loss patterns
Scarring alopecia is characterized by various patterns of hair loss, each with its unique manifestation. The most common patterns include:
- Patchy hair loss: This pattern appears as discrete areas of baldness on the scalp.
- Diffuse thinning: In some cases, scarring alopecia can lead to a diffuse thinning of hair across the entire scalp.
The progressive nature of scarring alopecia is a key feature of the condition. Over time, the affected areas may expand, resulting in a gradual decrease in hair density. This progressive nature can have a significant impact on the individual’s self-esteem and overall well-being.
Scalp inflammation and itching
Scalp inflammation and itching are frequently reported symptoms in individuals with scarring alopecia. The underlying inflammation can cause discomfort and irritation, leading to persistent itching. Scratching the affected areas can further exacerbate the inflammation and potentially result in secondary infections.
It is important to note that the discomfort associated with scalp inflammation and itching can have a profound impact on an individual’s quality of life. The constant urge to scratch can cause distress and disrupt daily activities, leading to psychological and emotional distress.
Changes in hair texture and appearance
Scarring alopecia can cause significant changes in hair texture and appearance. The affected hair may become:
- Thin
- Fragile
- Prone to breakage
Additionally, the hair may lose its natural shine and appear dull.
These changes in hair texture can be distressing for individuals, as they may feel self-conscious about the visible signs of hair loss. The emotional and psychological impact of these changes should not be underestimated, as they can affect self-esteem, body image, and overall confidence.
Diagnosis of Cicatricial Alopecia
A thorough medical history and physical examination play a crucial role in diagnosing scarring alopecia. The healthcare provider will inquire about the patient’s symptoms, duration of hair loss, and any relevant risk factors. A detailed examination of the scalp will be conducted to assess the pattern of hair loss, presence of inflammation, and any other visible abnormalities.
By gathering comprehensive information, healthcare providers can identify potential triggers or underlying conditions that may contribute to scarring alopecia. This aids in formulating an accurate diagnosis and developing an appropriate treatment plan.
Scalp biopsy and histopathology
Scalp biopsy is a definitive diagnostic procedure for scarring alopecia. During this procedure, a small sample of scalp tissue is extracted and examined under a microscope. Histopathological analysis allows for the identification of specific features associated with cicatricial alopecia, such as:
- Destruction of hair follicles
- Replacement of follicles with scar tissue
- Presence of inflammatory cells
The results of the scalp biopsy and histopathology provide valuable information to confirm the diagnosis of scarring alopecia and differentiate it from other types of hair loss.
Blood tests and laboratory investigations
In some cases, blood tests and laboratory investigations may be performed to rule out underlying causes or associated conditions that can mimic scarring alopecia. These tests may include:
- Complete blood count
- Thyroid function tests
- Autoimmune markers
- Hormonal assessments
It is important to note that while blood tests can be helpful in identifying potential contributing factors, they have limitations in directly diagnosing cicatricial alopecia. The diagnosis primarily relies on clinical evaluation, scalp biopsy, and histopathological findings.
Dermoscopy and trichoscopy
Dermoscopy and trichoscopy are non-invasive techniques that aid in the diagnosis and monitoring of scarring alopecia. These procedures involve the use of a specialized handheld device that magnifies the scalp and hair follicles, allowing for detailed examination.
Through dermoscopy and trichoscopy, specific findings and patterns can be observed, such as:
- Perifollicular erythema
- Follicular hyperkeratosis
- Follicular dropout
These findings can provide additional evidence to support the diagnosis of scarring alopecia and assist in monitoring the progression of the condition over time.
Treatment For Scarring Alopecia
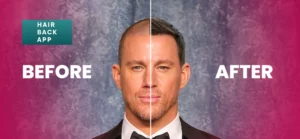
Hair transplantation techniques offer a promising solution for individuals suffering from scarring alopecia, providing a means to restore hair in areas affected by this condition. Hair transplantation techniques such as FUE Hair Transplant can be an option for individuals with this condition who have stable disease activity and healthy areas of hair-bearing scalp. This procedure involves the removal of hair follicles from the donor area, typically the back or sides of the scalp, and their transplantation into the affected areas.
However, it’s essential to note that scarring alopecia presents a challenge for hair transplantation because the scarred tissue may not support the growth of transplanted hair follicles effectively. Additionally, it can be a progressive condition, and the inflammation may persist even after the transplantation, potentially affecting the transplanted follicles.
Before considering hair transplantation for scarring alopecia, individuals should consult a dermatologist or a hair restoration specialist to assess the suitability of the procedure. A thorough evaluation of the condition and the extent of the scarring is necessary to determine whether hair transplantation is a viable option. Additionally, managing the underlying inflammatory process, if present, is crucial to improve the chances of successful transplantation and to prevent further hair loss in the transplanted areas.